Sep 7
/
Skillmed Institute
Decoding Female Pattern Hair Loss (FPHL)

Due to the ambiguous association between androgens and the presenting condition, female pattern hair loss (FPHL) has come to be the accepted terminology for androgenic hair loss in women. It is distinguished by a loss of hair density across the frontal scalp and crown, but the frontal hairline is retained.
From about 12% women between the ages of 20-29 to more than 50% women beyond the age of 80, the frequency rises with age. According to societal conventions, a woman's sexual orientation and sense of gender are fundamentally shaped by her hair, and any hair loss leads to feelings of low self-worth, depression and feeling of less appealing. (Fabbrocini et al., 2018)
Epidemiology
FPHL begins at a later age in women than in males. By age 29, 13% of women experience the onset of clinically identifiable FPHL; by age 49, 25%; by age 69, 41%; and by age 79, over 50% show some degree of FPHL. Only 43% of women 80 years and older do not exhibit any signs of FPHL. (van Zuuren et al., 2016)
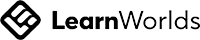
Sinclair Scale
- Stage 1: is typical. All females before puberty exhibit this pattern, whereas only 45% of women who are 80 years or older do.
- Stage 2: The centre part appears to be getting wider.
- Stage 3: The central section widens and the hair on each side of the core area thins.
- Stage 4: demonstrates the onset of scattered hair loss on the scalp's top.
- Stage 5: This represents severe hair loss. (Tosti et al., 2013)
Pathology And Pathogenesis Of FPHL
Male pattern hair loss (MPHL) and female pattern hair loss (FPHL) share the histological characteristic of hair follicle shrinkage and progressive vellus-like follicle development.
The cytochrome P450 enzyme 5-reductase converts testosterone into DHT, and aromatase then changes DHT into estrogen. On the basis of tissue distribution, substrate affinity, and pH maxima, two isoforms of 5'-reductase have been discovered and distinguished. DHT is assumed to be the major androgen responsible for hair loss. (Fabbrocini et al., 2018)
Clinical Features
Women experience gradual mid-frontal scalp thinning with rather sparse anterior hairline thinning. When the hair divides in the middle, the thinning becomes most noticeable, and the bare scalp might look like a Christmas tree.
After the commencement of adrenarche, hair loss can start at any age and can happen before pubarche and menarche.
Before any discernible decrease in hair volume, FPHL may first manifest as episodic or chronic hair losing. As an alternative, some women exhibit subtle crown thinning without noticing any increased hair loss. (Birch et al., 2002)
Before any discernible decrease in hair volume, FPHL may first manifest as episodic or chronic hair losing. As an alternative, some women exhibit subtle crown thinning without noticing any increased hair loss. (Birch et al., 2002)
Instead of baldness per se, a scalp examination reveals an enlargement of the center region and a generalized decline in hair density across the frontal scalp. There is often some indication of a general decrease in hair density across the scalp, even though certain locations exhibit the most pronounced decline in hair density.
The self-limiting condition known as acute telogen effluvia is frequently brought on by physical sickness, surgery, bleeding, or crash dieting. Chronic telogen effluvium (CTE) may appear as a result of iron deficiency anemia, systemic lupus, thyroid illness, drug use, and other conditions.
Inquiring about the patient's plans to conceive in the near future is particularly helpful because anti androgen medications have the potential to be teratogenic. Not every patient need blood tests for screening. It would make sense to check women for thyroid conditions, iron deficiency anemia, and hyperandrogenism suspicions before considering endocrinological screening. (Tosti et al., 2013)
Empty space, drag to resize
Comorbidities
Polycystic ovarian syndrome is the most typical endocrinologic comorbidity connected to FPHL. FPHL also seems to be often related with metabolic syndrome, which is defined by overweight, resistant to insulin, hypertension, hyperprolactinemia, and elevated aldosterone levels. (Birch et al., 2002)
Diagnosis
- Acute and persistent telogen effluvium (TE) ought to be taken into consideration in particular for women who have significant hair loss on mid-frontal scalp.
- The proper diagnosis requires an amneses and a physical examination.
- Any potential mental, emotional, or physical stresses that may have happened over the preceding three to six months should all be emphasized during anamnesis.
- Infertility, hirsutism, ovarian abnormalities, monthly irregularities, acne, and other hyperandrogenism-related symptoms should all be sought out during a history and physical examination.
- Rarely are the findings of laboratory tests reviewed in female patients with FPHL who do not exhibit hyperandrogenism. (van Zuuren et al., 2016)
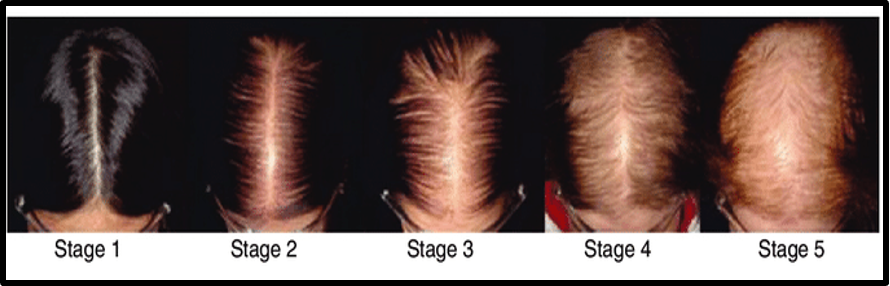
The precise form of female alopecia can be identified by hair analysis. Women have androgenetic alopecia in three phases. The findings of the hair testing will determine how many hairs are required to restore hair growth permanently.
Female androgenetic alopecia: The type of hair implants available will depend on the severity of the hair loss.
A thorough inspection of the hair will allow for an estimation of the required number of hairs and will suggest additional medical care based on either a static classification (Ludwig) or a more accurate multifactorial classification given by Dr. Pierre Bouhanna.
There will be three evaluation phases:
Stage 1:moderate thinning on the top of the head without reaching the frontal border.
Stage 2: open alopecia with short hair and located 1 cm behind the frontal line.
Stage 3: almost complete baldness with a thin band of hair at the forehead. (Bouhanna P, 2001)
Stage 2: open alopecia with short hair and located 1 cm behind the frontal line.
Stage 3: almost complete baldness with a thin band of hair at the forehead. (Bouhanna P, 2001)
Natural History
The rate of FPHL's advancement is widely diverse, but it is a progressive disorder in the absence of therapy. Hair loss occurs in spurts often. Before the shedding recovers to normal levels, women frequently feel significant hair loss every day in the shower or when brushing their hair for two to three months. It could take 3–12 months until the shedding starts over again. (Olsen et al., 2001)
Therapies
Minoxidil
Minoxidil topical solution is the only androgen-independent drug that is currently popular. According to the medication's theorized mechanism of action, telogen is prematurely terminated, anagen is likely prolonged, and hair cycling is affected. Although there are 2% and 5% formulations of this, only the 2% solution has FDA approval for FPHL at this time.
Typically, a dropper is used to apply 1 ml topical minoxidil twice day to a dry scalp. In order to enhance the medication's absorption, this is kept on for an hour before showering. Patients should be informed that a brief, self-limiting telogen effluvium may develop in the first 2–8 weeks.
Before a thorough assessment of effectiveness can be done, the course of treatment needs to be continued over at least 12 months. (Dinh et al., 2007).
Finasteride
Finasteride
The mechanism by which finasteride functions is to obstruct the 5-reductase II enzyme, which catalyzes the transformation of testosterone to the far more potent chemical 5 DHT. Finasteride inhibits total circulatory androgen activity, hence suppressing overall androgen activity. (Dinh et al., 2007).
Cyproterone Acrylate
This drug blocks androgen receptors and suppresses gonadotropin-releasing hormone (GnRH). Cancer of the prostate, hirsutism, and chronic acne are among further indications. It is frequently used in Australia in the oral contraceptive medication Diane-35, which also contains estradiol.
Menstrual irregularities, weight gain, libido loss, depression, nipple tenderness, and digestive issues are among the list of adverse effects. (Dinh et al., 2007).
Flutamide
Flutamide is an effective androgen antagonist that works by blocking androgen receptors. As a result, it is frequently utilized to treat hirsutism and advanced prostate cancer. (Dinh et al., 2007).
Hair Transplantation
When hair loss has stabilized and people with FPHL over the age of 25 have tried medicinal therapy without success, transplantation of hair is a viable alternative. Hairs located in the occipital region are moved or transferred to the bald area during hair transplantation.
Women who have significant hair loss or frontal scalp thinning and good hair density over the occipital area make excellent surgical applicants for hair transplantation. (van Zuuren et al., 2016)
Follicular unit transplanting hair is a surgical procedure used to cure baldness. To achieve a natural appearance, follicular units of hair, which naturally form bundles of hair, undergo dissection under a stereomicroscope.
One session of the treatment, which is carried out under local anesthetic, entails the transplanting of 800 – 1200 grafts. Follicular unit transplantation has greatly reduced the amount of invasiveness of the procedure while still producing natural-looking, undetectable, and repeatable outcomes. (Olsen et al., 2001).
Conclusion
Effective management of the condition requires a deep understanding of its possible underlying factors, any coexisting health conditions, potential diagnostic options, and the various available treatment modalities.
Furthermore, it necessitates empathetic communication with patients and heightened awareness. Failure to administer appropriate medication could lead to a deterioration in the patient's condition.
Furthermore, it necessitates empathetic communication with patients and heightened awareness. Failure to administer appropriate medication could lead to a deterioration in the patient's condition.
The current medical approach not only halts further progression but may also stimulate partial regrowth. Regardless of the specific medication employed, both the patient and the healthcare provider must exhibit patience and perseverance due to the gradual nature of the treatment response.
References
Fabbrocini, G., Cantelli, M., Masarà, A., Annunziata, M. C., Marasca, C., & Cacciapuoti, S. (2018). Female pattern hair loss: A clinical, pathophysiologic, and therapeutic review. International journal of women's dermatology, 4(4), 203-211. https://www.sciencedirect.com/science/article/pii/S2352647518300224
Birch, M. P., Lalla, S. C., & Messenger, A. G. (2002). Female pattern hair loss. Clinical and experimental dermatology, 27(5), 383-388. https://academic.oup.com/ced/article-abstract/27/5/383/6626100
Bouhanna, P. (2001). Multifactorial Classification of Male and Female Androgenetic Alopecia. Dermatologic Surgery, https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1524-4725.2000.00009.x
Dinh, Q. Q., & Sinclair, R. (2007). Female pattern hair loss: current treatment concepts. Clinical interventions in aging, 2(2), 189-199. https://www.tandfonline.com/doi/abs/10.2147/ciia.S12159900
Dinh, Q. Q., & Sinclair, R. (2007). Female pattern hair loss: current treatment concepts. Clinical interventions in aging, 2(2), 189-199. https://www.tandfonline.com/doi/abs/10.2147/ciia.S12159900
Herskovitz, I., & Tosti, A. (2013). Female pattern hair loss. International Journal of Endocrinology and Metabolism, 11(4). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3968982/
Olsen, E. A. (2001). Female pattern hair loss. Journal of the American Academy of Dermatology, 45(3), S70-S80. https://www.sciencedirect.com/science/article/pii/S0190962201867487
Van Zuuren, E. J., Fedorowicz, Z., & Schoones, J. (2016). Interventions for female pattern hair loss. Cochrane Database of Systematic Reviews, (5). https://research.bangor.ac.uk/portal/en/researchoutputs/interventions-for-female-pattern-hair-loss(cf592236-b21f-41f0-88c9-ae4b284fe3d8).html

Company
Need Help?
Recruitment
Made in Europe ©2024 Skillmed